 Dear Colleague:
Dear Colleague:
This winter is off to an exciting start with the CDC’s release of recommendations for use of the new 12-dose regimen for the treatment of latent TB infection. This issue of the Northeastern Spotlight includes a short article about the new regimen, as well as where you can go to learn more about it. The short-course treatment recommendations were also an unanticipated highlight at the West Virginia TB Symposium on December 8th & 9th, which you can read about below. And continuing in this theme, this installment in the behavioral/social science series looks at research dissemination. It remains to be seen how adoption and implementation of 12-dose regimen will unfold, but it is certainly exciting to have another treatment option available.
The new regimen is not the only exciting event in the world of TB. Dr. James Sunstrum, TB Medical Consultant for the State of Michigan, shares his work in the Great Lakes State and beyond in this issue. Born There, a poem by Dr. Curi Kim about a passenger with MDR-TB who arrived at the Detroit airport from Africa, provides a lyrical look at what Dr. Sunstrum describes as the most challenging TB case of his professional career.
Two helpful resources—archived webinars and the cultural competency newsletter—are available on our website, and in this issue you’ll find more information about them. We also give you a look at our 5th Annual TB Medical Consultants’ Meeting, which was held in November.
Finally, a reminder that World TB Day is just around the corner. CDC’s slogan for this year’s event is “Stop TB in my lifetime,” and with each new advance in testing and treatment this goal slowly becomes more attainable.
Lee B. Reichman, MD, MPH
Executive Director
Northeastern RTMCC and the
Global Tuberculosis Institute
back to top
Behavioral/Social Science Article On Research Dissemination
The worlds of research and practice have long suffered from a form of disconnect – innovative behavioral approaches only enter routine practice many years after their efficacy results have been published in academic journals. Contributing to the delay, few reports of efficacious interventions discuss how they may be successfully implemented in diverse settings and how implementation may be assessed to determine fidelity to the intervention as it was empirically validated.1,2 An oft-quoted but rarely cited statistic suggests that it takes an average of 17 years for a proven medical intervention to be implemented in clinical practice.3
Research Dissemination in TB
The CDC-funded Tuberculosis Epidemiologic Studies Consortium (TBESC) was founded with a mandate to conduct epidemiologic, behavioral, economic, and operations research.4 Because of the emphasis on making TBESC research relevant to TB control programs, it was decided in the early years of the Consortium to convene a group specifically to disseminate research results – the Translating Research into Practice (TRiP) workgroup.
TRiP influences TBESC activities in several ways. Protocol teams proposing new projects (called “Task Orders”) are required to suggest specific activities for disseminating results. These ideas are reviewed in progress reports prepared each six months by Task Order investigators. Upon study completion, TRiP members work with each Task Order investigator to plan and implement specific dissemination activities, with input from representatives of the Regional Training and Medical Consultation Centers.
Dissemination has focused both on study findings and on materials developed in the research process. In the latter case, this includes manuals, guides, slide sets and videos related to training, formative research, study implementation, and program evaluation. These materials may be accessed online at http://www.findtbresources.org/trip.aspx.
Methods for disseminating study findings go beyond the traditional methods of conference presentations and publication in the academic literature. Task Order 4 (“Models for incorporating HIV counseling, testing, and referral into TB contact investigations”) results were shared in a Fact Sheet that accompanied a Dear Colleague letter from CDC Division of TB Elimination (DTBE) Director Dr. Kenneth Castro to all TB controllers.
Results from Task Order 9 (“Missed opportunities for TB prevention in foreign-born populations in the US and Canada”) fed into the process of developing new CDC Guidelines for serving foreign-born patients. Other Task Orders such as Task Order 11 (“Addressing TB among African-Americans in the Southeast”) have been or will be featured in TB Notes, a newsletter distributed by DTBE to TB controllers and others involved in national TB programs.
Other Research Dissemination Efforts
In the early years of the battle against HIV/AIDS , a number of researchers working independently developed wide-ranging behavioral and educational interventions to prevent HIV transmission. It soon became clear that a centralized mechanism for identifying and disseminating effective, innovative interventions was essential. Accordingly, CDC initiated the Diffusion of Effective Behavioral Interventions (DEBI) project. Interventions which have proven by objective criteria to be effective in accomplishing certain HIV prevention goals with given population groups are evaluated and then publicized through the DEBI website (http://www.effectiveinterventions.org/en/home.aspx). To date, the website lists 29 interventions, along with 3 public health strategies, for which they offer training through a national network of STD/HIV Prevention Training Centers. The CDC also maintains a Compendium of Evidence-Based HIV Behavioral Interventions (http://www.cdc.gov/hiv/topics/research/prs/compendium-evidence-based-interventions.htm). At the current time, this website lists 74 HIV risk reduction evidence-based behavioral interventions, 68 of which are individual-level and group-level interventions and 6 are community-level interventions. Further, these interventions are divided into Best-evidence (44) and Good-evidence (30) interventions
Finally, the federal Substance Abuse and Mental Health Services Administration (SAMHSA) keeps an on-line searchable listing of effective substance abuse and mental health interventions, called the National Registry of Evidence-Based Programs and Practices (NREPP). At the current time, NREPP contains information on 220 interventions (http://www.nrepp.samhsa.gov/).
The Development of Implementation Research
Systematic investigation of how programs are implemented is increasingly seen as an essential arm of behavioral health research.2,5,6 For example, the second phase of the President’s Emergency Plan for AIDS Relief is promoting an implementation science approach in an effort to improve program effectiveness in “real-world” settings.7
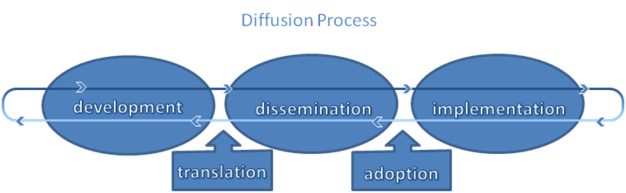
SAMHSA’s Addiction Technology Transfer Center (ATTC) Network has developed materials which illustrate how evidence-based practices developed through research may be utilized. The ATTC posits a process of five major stages in the Diffusion Process:
1) Development: the creation and initial evaluation of an innovation, be it an idea, technology, treatment or method;
2) Translation: definition of an innovation’s essential elements and relevance, followed by preparation for dissemination;
3) Dissemination: promotion of an innovation to facilitate adoption and implementation. This may involve raising awareness, building knowledge, and distributing materials;
4) Adoption: the process of deciding whether or not to use an innovation; and
5) Implementation: incorporation of an innovation into routine practice, ideally with a range of strategies to address individual, organizational, and systemic characteristics (e.g., skills training, administrative buy-in, and policy changes).
The following graphic represents this process. The horizontal looping arrows are meant to represent the process’ bi-directionality. The diffusion of an innovation is an iterative process where practices are shaped by their use in real-world settings, resulting in changes which are then evaluated through research (http://www.attcnetwork.org/explore/priorityareas/techtrans/techtransfer/).
Future Directions
In an effort to facilitate an accelerated and systematic process for the translation, dissemination, and implementation of evidence-based practices, the National Institutes of Health in 2004 launched its “NIH Roadmap for Medical Research” initiative. This initiative is meant to transform biomedical research by filling defined knowledge gaps and addressing roadblocks to research. These efforts focus on two stages of translating research for clinical practice: “T1” which addresses moving research findings in the laboratory into clinical practice (often called “bench to bedside”), and “T2” where research findings using rigorous designs (randomized controlled trials, etc.) are moved into routine practice in the community. Perhaps between these new funding streams and increased attention to dissemination and implementation research, the 17-year lag between research and routine practice may finally be reduced.
Submitted by Paul Colson, PhD, Program Director,
And Julie Franks, PhD, Health Educator and Evaluator,
Charles P. Felton National TB Center, ICAP, Columbia University.
1 Mowbray CT, Holter MC, Teague GB, Bybee D. Fidelity criteria: development, measurement, and validation. American Journal of Evaluation 24(3):315-340. 2003.
2 Proctor EK, Landsverk J, Aarons G, Chambers D, Glisson C, Mittman B. Implementation Research in Mental Health Services: an emerging science with conceptual, methodological challenges. Administration and Policy in Mental Health 36:24-34. 2009.
3 Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yearbook of Medical Informatics. National Library of Medicine, Bethesda, MD:65-70. 2000.
4 Katz D, Albalak R, Wing JS, Combs V. Setting the agenda: a new model for collaborative tuberculosis epidemiologic research. Tuberculosis 87:1-6. 2007.
5 Cohen DJ, Crabtree BF, Etz RS, Balasubramanian BA, Donahue KE, Leviton LC, Clark EC, Isaacson NF, Stange KC, Green LW. Fidelity versus flexibility: translating evidence-based research into practice. American Journal of Preventive Medicine 35(5S):S381-S389. 2008.
6 Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R, Hensley M. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health 38:65-76. 2011.
7 Padian NS, Holmes CB, McCoy SI, Lyerla R, Bouey PD, Goosby EP. Implementation science for the US President’s Emergency Plan for AIDS Relief. Journal of Acquired Immune Deficiency Syndrome 56(3):199-203. 2011.
back to top
Profile: James Sunstrum, MD, TB Consultant for the State of Michigan and Medical Director for the Wayne County TB Clinic
Dr. James Sunstrum, TB Consultant for the State of Michigan and Medical Director for the Wayne County TB Clinic, became involved with TB by complaining. Originally from western Canada, after completing medical school in Saskatchewan he moved to Michigan to do an internship, and has practiced as an infectious disease physician there ever since. Working at a local hospital in 1995, he began to see TB patients being readmitted to the hospital. “I realized the local TB clinic wasn’t up-to-date, and I complained to my local health department about the poor management of TB patients,” Dr. Sunstrum recounted. “The health department responded by asking me to come and run the county TB clinic, and I’ve been involved with TB ever since.”
This pattern repeated itself a couple years later when an outbreak in an illegal undocumented men’s “shelter” resulted in about fifteen active TB cases and one death. “I made another complaint to the Michigan Department of Community Health that there weren’t enough local resources available to deal with this outbreak—the health department was totally overwhelmed, so the state came to help close down the shelter and provide some support. But they realized they did not have a state TB medical consultant, and they asked me to do that job as well.” On a related note, Dr. Sunstrum must lodge extremely amiable complaints if he ended up with two job offers out of it.
The TB clinic Dr. Sunstrum practices at is in Westland, which is very close to Detroit Metropolitan Airport. “I got a call from CDC one morning in the early ‘90s asking if I would be willing to go to the airport if they ever saw a suspected case of bubonic plague from India, and I said sure.” Fortunately he never saw a case of bubonic plague, although once the airport reported a suspected case of Ebola Virus. “I had to quickly go out there, and thankfully it was nothing like Ebola—just a woman with a rash. But we had to quickly deescalate the situation and sort things out.”
Dr. Sunstrum’s most professionally challenging case involved a man who had flown from Africa to Detroit with contagious MDR-TB. “The man knew he had TB—there were MDR-TB drugs in his luggage—and he knew he wasn’t getting any better in Africa so he bought a plane ticket to the US. We took him straight to the hospital and he stayed there for nine months. It was very complicated medically because of all the drugs we had to give him. It was also very complex legally because he was only allowed into the US for medical humanitarian reasons, so immigration was waiting to deport him. He had applied for asylum, so after he was finally released from the hospital he was held in an immigration jail while he went through immigration proceedings., Eventually he was deported back to Africa with enough drugs to complete his treatment. Thankfully this was the most complicated patient we’ve ever had come from the airport.”
In his spare time, Dr. Sunstrum enjoys sailing a Laser, a type of one-man sailboat. He became interested in sailing while growing up in Sascatchewan, where windy conditions made it both difficult to control the boat and fun because you could build up a lot of speed. Cycling is another hobby, and bike paths are slowly becoming more common in southeast Michigan.
Dr. Sunstrum has also been on two volunteer trips to Uganda to train doctors, first in 2009 to teach a three week course about modern principles of HIV care, and again in 2011 for an HIV/TB training course. “The neat thing about the TB clinic I was working at was that it was outdoors on a patio, next to an HIV clinic that would see 200 patients each morning. Every patient is screened for TB symptoms on every visit. Those who had some sort of TB symptoms would be pulled aside and sit on the patio, and we’d sit there with our laptops with our wireless network and we could do sputums and whatnot out there.”
During his time in Uganda, Dr. Sunstrum came to appreciate just how vital laboratory support is for the diagnosis and management of TB. “They had microscopy smears, and that was it. They had recently obtained a GeneXpert machine in Uganda when I was there, and they were training the technicians on how to use it. In three to five years the diagnosis of TB in these countries might be done quite differently from the way it’s currently done. One thing I noticed is that the diagnosis of HIV is crystal clear and very precise and accurate, but when you don’t have very good lab support the diagnosis of TB is vague and fuzzy. It’s just this cloudy thing that might be TB, could be TB. I saw many people at the HIV clinic who were put on TB therapy mostly because of an educated guess. It’s really tough for the doctors. If you fail first line drugs, you’re retreated with first line drugs, and then if you fail again you’re treated with second line drugs. It’s done strictly on clinical pathways, with the absence of any laboratory confirmation. The man who came to Michigan in the plane had been on second line drugs, but it was all guess for the clinicians in Africa. They didn’t have any lab confirmation and they were only half-right in making their guesses. I think we are completely unprepared for the quantity of MDR-TB coming out of these countries.”
Fortunately in Uganda there was a good supply of both TB and HIV medications. But as Dr. Sunstrum pointed out, “It’s one thing to have access to these medications, but you also have to teach these doctors how to properly use them, which was what I did while I was there,” Dr. Sunstrum said. “It’s a topic that interests me quite a bit, and I hope I can continue going back every one or two years.”
Even back in Michigan, Dr. Sunstrum comments that he’s still plenty involved in international issues. “Two-thirds of our patients here originally come from overseas. It’s one of the most ethnically diverse experiences you can get in a morning clinic! I have a map of the world on my wall, and if I see a patient with active TB I put a pin on the map. Southeast Michigan has the highest proportion of Middle Eastern immigrants in the whole United States, so I have lots of pins in Lebanon, Yemen and Iraq.”
One of Dr. Sunstrum’s favorite stories to tell his clinic patients is a personal one: While in medical school, he was exposed to a TB patient who went undiagnosed for two weeks, and he personally ended up with latent TB. “It’s a very effective story when talking with patients about taking treatment for latent TB, and the recommendation of taking medications the same as I did in the past.” Whether it’s his local health department, doctors in Uganda, or patients in his clinic, Dr. Sunstrum is ready to lend a helping hand.

Dr. Sunstrum (top right, with glasses) with physicians he was training in Uganda
Submitted by
Nickolette Gaglia, MPH
Training and Consultation Specialist
NJMS Global Tuberculosis Institute
back to top
Born There—A Poem
Born There
Birth geography
Tied tight to longevity
But when might is right
What rights are given that might
Right the balance of the world
No rites can heal this
Hideous hemoptysis
If a mite of care
The mighty felt to fight white
Plague, then this I needn’t write
About the poem
This poem was inspired by a patient with Multi-Drug Resistant Tuberculosis who arrived on a plane at Detroit Metropolitan Airport from Africa, and the dedication of colleagues to cure him. He would otherwise have died, another statistic in an epidemic of injustice.
This case is also discussed in this issue’s profile piece on Michigan TB Medical Consultant Jim Sunstrum.
Reprinted from Online Journal of Health Ethics Vol 7, No 2, November 2011
Submitted by
Curi Kim, MD, MPH
Medical Officer
Division of Global Migration and Quarantine
US Centers for Disease Control and Prevention
back to top
Archived Webinars Available on GTBI Website
Have you wanted to view a particularly interesting webinar but a time conflict prevented you from participating? GTBI records and posts many of its webinars online for later viewing. The archive page, located at http://globaltb.njms.rutgers.edu/educationalmaterials/audioarchives.html, extends back to 2006 and includes over 20 of our most popular webinars as well as links to supplemental materials mentioned during the presentations. This is also a great resource for educating new staff or for viewing as a group during staff meetings.
Our most recent archived webinars include:
Treatment of TB: Managing Adverse Drug Effects
http://globaltb.njms.rutgers.edu/educationalmaterials/audioarchives.html
This web-based seminar discusses the management of medication side effects in TB patients to decrease the risk of toxicity and ensure completion of therapy.
Medical Update: Diagnosis and Management of Tuberculosis in the Pregnant Patient
http://globaltb.njms.rutgers.edu/educationalmaterials/audioarchives.html
This web-based seminar covers screening, diagnosis, treatment, and management of TB patients who are pregnant.
Best Practices in TB Control: Cohort Review Series
#1: Introduction to the TB Cohort Review Process
http://globaltb.njms.rutgers.edu/educationalmaterials/audioarchives.html
#2: Key Activities and Roles in the TB Cohort Review Process
http://globaltb.njms.rutgers.edu/educationalmaterials/audioarchives.html
#3: TB Cohort Review in Action: Putting it all Together
http://globaltb.njms.rutgers.edu/educationalmaterials/audioarchives.html
The purpose of these web-based seminars is to provide TB program leaders, managers, clinicians and case managers with the necessary knowledge and skills to participate in TB cohort reviews in their program areas.
back to top
TB and Cultural Competency: An Ongoing Exploration
In 2004, GTBI released the first issue of a new newsletter, TB and Cultural Competency–Notes from the Field. This printed and online newsletter was intended as a companion piece to our booklet, Cultural Competency and Tuberculosis Care: A Guide for Self-Study and Self-Assessment. While the guide describes the general principles of cultural competency and includes tools for self assessment, the newsletter highlights real-life examples of how culture plays a role in the diagnosis, treatment, and management of TB. Each issue includes a case presentation with articles and resources to support the teaching points from the case. Cases highlight challenges encountered and successful approaches utilizing the core principles of cultural competency. The cases are identified from TB programs throughout the United States. Over the last eight years, some of the topics explored in the newsletter include patient centered care, stigma, use of interpreters and health beliefs, migrant workers, and refugees. The newsletter explores culture in terms of ethnic identify as well as in the larger sense. Highlighted cases have included patients from Korea, Mali, Ecuador, and Burma among others as well as those from the culture of methamphetamine use, and those receiving a dual TB/HIV diagnosis.
The recently released Winter 2011 issue, No Woman is An Island, explores the challenge of providing care within the context of an immigrant community and describes one health care worker’s experience as she established a relationship with a patient and the larger community. This issue, as well as all past issues, can be accessed here. We are always looking for cases to highlight, so if you or a colleague have worked with a TB patient where culture played a role, please let us know. This could be a case that was challenging due to your patient’s cultural beliefs or practices being dissimilar from your own, or a case where you experienced success because you changed your typical approach based on something you learned about the patient’s culture. We’d love to highlight your case in an upcoming issue, so let us know if you have a case to share with your fellow health care workers in the Northeast!
Submitted by Nisha Ahamed, MPH, CHES
Director of Education & Training
NJMS Global TB Institute
back to top
Breaking News at the West Virginia TB Symposium
In a wood-paneled lodge overlooking snowy Stonewall Jackson Lake State Park, nearly a hundred attendees gathered in early December for the West Virginia TB Symposium. The symposium began at noon on December 8th in order to allow attendees time to drive there in the morning, and ended at 12:45 the next day. A dinner for all attendees on the first night allowed time to mingle with faculty, and gave those gathered a chance to network with colleagues they don’t frequently see in person due to the large size of the state.
The symposium, jointly sponsored by the West Virginia Division of TB Elimination and GTBI, featured presentations highlighting the TB work being done in the state, as well as touching on historical and emerging topics related to TB control. The symposium began with an engaging look at the history of TB by Dr. Dominic Gaziano, Medical Director of the West Virginia Division of TB Elimination. His son, Dr. Michael Gaziano, followed with an exploration of why TB rates are declining in the United States. Dr. Alfred Lardizabal of GTBI presented on TB targeted testing and risk assessment, and underscored the need for a risk assessment before deciding to test for latent infection. Dr. David Holland, Professor at Duke University and Assistant Medical Director of the North Carolina TB Control Program, rounded out the first day with a look at LTBI treatment modalities and completion of therapy. Dr. Holland was checking his email about four hours before his presentation when he saw that CDC had released the 12-dose regimen for LTBI treatment (3HP) study results and guidelines. He updated his slides to include this late-breaking information, and it was a special treat for everyone in the audience to hear about this new from such an expert!
The second day focused primarily on TB in West Virginia, and began with Dr. Gregory Juckett of West Virginia University Student Health Services sharing his experiences with TB in Colleges and Universities. Dr. Krista Powell, an EIS Officer with CDC, discussed her work with an outbreak in federal prisons located in West Virginia, offering an intriguing look into the complexities of tracing contacts after they’ve been transferred to other facilities. Dr. Harry Tweel of Greenbrier County Health Department gave an overview of TB and co-morbidities, and the day was rounded out by five illustrative case presentations by Public Health Nurses in West Virginia, followed by a panel discussion. Attendees noted on their evaluations that they particularly enjoyed the case presentations and panel discussion because it allowed those gathered an opportunity to discuss the challenges they face and learn from those who had been in similar situations.
We thank the West Virginia Division of TB Elimination, especially Carmen Priddy, Barbara Simpkins, Libby Boggess , Joyce Brown, Brice Fortney, Linda Winkle, Dr. Dominic Gaziano, Kala Burgett, Toby Waggoner, and Loretta Haddy for their vision and hard work that made this event such a success. On their evaluations, attendees frequently commented that they wished this conference was held more frequently, and we look forward to collaborating with West Virginia again in the future.
Submitted by
DJ McCabe, RN, MSN
Trainer and Consultant, Clinical Programs
NJMS Global Tuberculosis Institute
Nickolette Gaglia, MPH
Training and Consultation Specialist
NJMS Global Tuberculosis Institute
5th Annual TB Medical Consultants Meeting: Exploring New Challenges and New Solutions
The Global Tuberculosis Institute held its 5th Annual TB Medical Consultants Meeting on November 9-10, 2011. Attendees included medical consultants from 18 project areas within the Northeastern United States. This meeting is provided for consultants annually, in order to support ongoing clinical consultation services, enhance program collaboration to share resources and expertise, as well as to update attendees on new treatment modalities. This year's meeting began with keynote speaker Anne Fanning, MD, Professor Emeritus at the University of Alberta, Canada, who addressed both local and global challenges towards the elimination of TB. The other plenary sessions explored pertinent and compelling topics from outside the "TB community," including TB in Emergency Department Settings, Diagnosis and Management of TB in the Pregnant Patient, and Management of TB in Patients on TNF-Alpha Antagonists. This was followed by an interactive panel discussion. At the conclusion of the first day, participants attended a networking social and dinner. This provided a collegial setting with much discussion about current challenges being faced in TB.
The second day of the meeting was held at the Global Tuberculosis Institute and featured several interactive case presentations with discussions, including participation in a TB Expert Network Conference hosted by CDC – Division of TB Elimination. In addition, Dr. Sundari Mase, CDC – Division of TB Elimination, provided a national overview of the RTMCC medical consultation system. Dr. John Jereb, CDC – Division of TB Elimination, reviewed findings from the TB Trials Consortium PREVENT TB Study of the twelve dose weekly regimen of isoniazid (INH) and rifapentine (RPT) for the treatment of LTBI. This study was the basis for the recent CDC recommendations on the twelve dose regimen for the treatment of LTBI, which is a combination regimen of Isoniazid and Rifapentine (3HP) given in twelve once–weekly doses under directly observed therapy (DOT). Time was also set aside for participants to share complex TB cases, which led to valuable discussion and participation by all attendees. Overall, the meeting was a success, with participants stating that they found the meeting very helpful, enjoyed the free dialogue, and that they are looking forward to next year's meeting!
Submitted by
Alyce Caulfield, MPH
Research Associate III
NJMS Global Tuberculosis Institute
back to top
CDC Issues Recommendations for Shorter Treatment Regimen for Latent TB Infection
On December 9, 2011, the US Centers for Disease Control and Prevention released guidelines in Morbidity and Mortality Weekly Report for a shorter treatment regimen for latent TB infection. This new regimen, called the 12-dose regimen and also sometimes referred to as 3HP, reduces treatment to 12 once-weekly doses given over 3 months.
The 12-dose regimen comes after a large randomized control trial found a combination of isoniazid (INH) and rifapentine (RPT) administered in 12 once-weekly doses as directly observed therapy (DOT) was as effective in preventing TB as the 270-dose INH regimen, which is usually self-administered by patients daily over nine months. Two other smaller studies have also found the 12-dose INH and RPT regimen to be as effective as other regimens. The 12-dose regimen also had greater rates of completion than the U.S. standard regimen of nine months of INH daily.
The 12-dose regimen should be administered under DOT to ensure the completion of all doses. Patients also need to undergo monthly clinical monitoring that includes inquiries about side effects and a physical assessment for signs of adverse events. DOT workers should be trained on how to educate patients about adverse effects and how to inquire about symptoms.
This new regimen does not replace existing treatment options for latent TB infection, but is another option for treatment in otherwise healthy people, 12 years of age and older, who were recently in contact with someone who has TB, or who tested positive for TB infection.
According to CDC, additional studies are needed to confirm efficacy and safety before this new treatment can be recommended in certain groups of people, including young children and people infected with HIV who are taking antiretroviral therapy. These people should be treated with other existing treatment regimens.
More than 11 million people living in the United States have latent TB infection, and about 5 to 10 percent (550,000 to 1.1 million) of those infected with TB in the United States will develop TB disease if not treated. Some people with weakened immune systems, like those with HIV and people with diabetes, are more likely to develop TB disease after infection.
Treating latent TB infection so it does not progress to TB disease is a cornerstone of the U.S. strategy for TB elimination. “Achieving TB elimination in the United States means not only treating people who already have TB disease, but also successfully treating people with latent TB infection who are at high risk for developing TB disease and potentially transmitting it to others,” says Dr. Kenneth Castro, Director of the Division of Tuberculosis Elimination at CDC.
The full recommendations for the new 12-dose regimen are available here: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6048a3.htm?s_cid=mm6048a3_w
back to top
Medical Consultation
GTBI faculty and staff respond to requests from providers seeking medical consultation through:
- Our toll-free TB Infoline: 1-800-4TB-DOCS and
- Email
During each consultation, the GTBI consultants will advise providers of TB Program resources for consultation in their jurisdiction. In addition, TB programs will be informed of TB cases with public health implications such as MDR/XDR-TB, pediatric TB in children <5, or potential outbreak situations.
More information about our consultation service, including downloadable Core TB Resources, can be accessed at Medical Consultant Web-Based Grand Rounds (http://www.umdnj.edu/globaltb/consultation.htm).
Periodically, designated TB program medical consultants are invited to participate in a web-based TB case conference (or grand rounds). Consultants are encouraged to present challenging TB cases on which they would like feedback from their colleagues throughout the Region. The next grand rounds will be held this Fall and we will notify TB programs when a date and time have been established. TB program medical consultants who would like to present a case should contact Dr. Alfred Lardizabal at 973-972-8452 or lardizaa@umdnj.edu.
back to top
Upcoming NE RTMCC Training Courses
Courses are open to participants in the 20 project areas (Maine, New Hampshire, Vermont, Massachusetts, Rhode Island, Connecticut, NJ, New York State, New York City, Pennsylvania, Michigan, Indiana, Ohio, West Virginia, Delaware, Maryland, Washington DC, Detroit, Baltimore, and Philadelphia) which are served by the Northeastern National Tuberculosis Center.
Individuals outside of this region who wish to attend our training courses should first contact their Regional Training and Medical Consultation Center to check if a similar course is being offered. If this is not the case, the out-of-region participant may then register for this course.
Click here for the list of upcoming courses.
back to top
Links - Other TB Resources
Division of Tuberculosis Elimination
The mission of the Division of Tuberculosis Elimination (DTBE) is to promote health and quality of life by preventing, controlling, and eventually eliminating tuberculosis from the United States, and by collaborating with other countries and international partners in controlling tuberculosis worldwide.
Find TB Resources Website
This website provides a central, comprehensive searchable database of international, national, state, and local TB-related education and training materials for TB healthcare workers, health professionals, patients, and the general public. Users can also submit their education and training materials as well find information on funding opportunities, TB organizations, TB mailing lists, and TB images.
TB Education & Training Network (TB ETN)
The TB Education and Training Network (TB ETN) was formed to bring TB professionals together to network, share resources, and build education and training skills.
Regional Training and Medical Consultation Centers' TB Training and Education Products
This website provides a searchable list of all 4 RTMCCs' resources.
TB-Related News and Journal Items Weekly Update
Provided by the CDC as a public service, subscribers receive:
- A weekly update of TB-related news items
- Citations and abstracts to new scientific TB journal articles
- TB conference announcements
- TB job announcements
- To subscribe to this service, click here
TB Behavioral and Social Science Listserv
Sponsored by the DTBE of the CDC and the CDC National Prevention Information Network (NPIN), this Listserv provides subscribers the opportunity to exchange information and engage in ongoing discussions about behavioral and social science issues as they relate to tuberculosis prevention and control.
Other RTMCCs
The Curry International Tuberculosis Center serves: Alaska, California, Colorado, Hawaii, Idaho, Montana, Nevada, Oregon, Utah, Washington, Wyoming, Federated State of Micronesia, Northern Mariana Islands, Republic of Marshall Islands, American Samoa, Guam, and the Republic of Palau.
The Heartland National Tuberculosis Center serves: Arizona, Illinois, Iowa, Kansas, Minnesota, Missouri, New Mexico, Nebraska, North Dakota, Oklahoma, South Dakota, Texas, and Wisconsin.
The Southeastern National Tuberculosis Center serves: Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia, Puerto Rico, and the U.S. Virgin Islands.
back to top
Key Contacts
- Lee B. Reichman, MD, MPH - Executive Director
- Reynard J. McDonald, MD - Medical Director
- Bonita T. Mangura, MD - Director of Research
- Eileen C. Napolitano - Deputy Director
- Nisha Ahamed, MPH, CHES - Program Director, Education and Training
- Nickolette Gaglia - Northeastern Spotlight Editor
- Alfred S. Paspe - User Support Specialist/Webmaster
back to top











